telehealth (telemedicine)
What is telehealth (telemedicine)
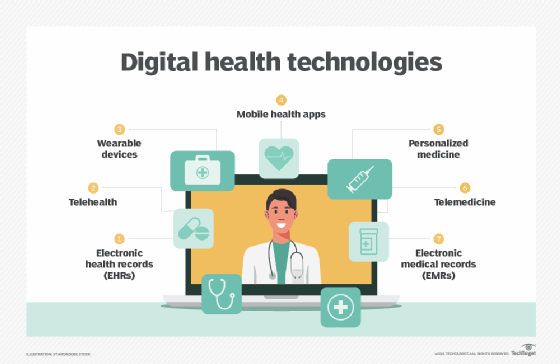
Telehealth, also referred to as telemedicine or e-medicine, is the remote delivery of healthcare services over the telecommunications infrastructure.
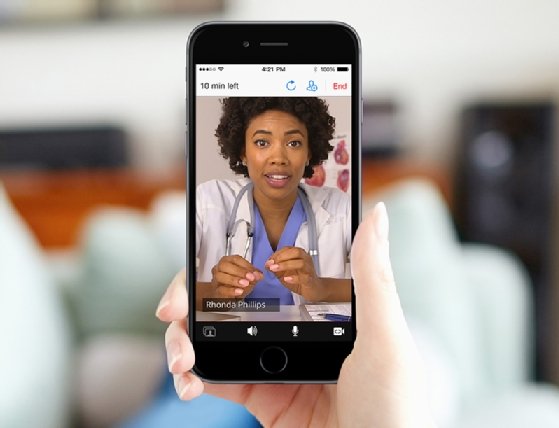
Telehealth allows healthcare providers to evaluate, diagnose, inform and treat patients without an in-person visit. Patients can communicate with physicians from their homes using their own personal technology or by visiting a dedicated telehealth kiosk.
A typical telehealth exam involves downloading an application or calling a telehealth number, provided by a physician's office or patient's employer as part of health insurance benefits. After sharing information about medical history and symptoms, the remote patient will be connected to a clinician. Based on the clinician's evaluation, the call will end with the patient receiving further instructions, such as what over-the-counter or prescription medication to take, and whether they need a follow-up appointment.
Types of telehealth
Telehealth can be classified into four main categories that in some cases overlap.
- Interactive. Physicians and patients communicate in real time from patient's home or a designated medical kiosk. They can interact using phones or videoconferencing software that complies with the Health Insurance Portability and Accountability Act regulations.
- Remote patient monitoring. Telemonitoring lets patients monitor symptoms or their condition from their home. They use mobile health devices, such as wearable technology, and applications that collect data about temperature, blood sugar levels, blood pressure and other vital signs.
- Store and forward. Also known as asynchronous telehealth, this approach lets one healthcare provider share patient information, such as lab results, with another healthcare provider.
- Mobile. Mobile telehealth describes healthcare activities supported by mobile devices. This could be remote clinical services, such as consultations, and patient-doctor communication through mobile patient portals. It can also include public health activities, such as disseminating warnings about a dangerous outbreak.
Advantages of telehealth
Some of the benefits of telehealth for patients include the following:
- Convenience. Patients don't have to take time away from work for an appointment, and they save travel time and associated expenses, such as paying for gas and childcare. This can be useful for minor medical needs that don't require urgent care and for routine check-ins for patients with chronic conditions.
- Increased access. Patients in rural areas can obtain specialty health services, such a mental health treatment and post-surgery follow up, that they otherwise might not get without traveling a long distance for an in-person visit. Similarly, patients who live in federally designated underserved areas have increased access to primary, dental and mental healthcare. Patients who are unable to travel to an appointment because of their health condition can also receive care they might not otherwise get.
- Reduced exposure. Telehealth allows sick people to get healthcare without the risk of infecting others or becoming infected themselves.
Telehealth also provides advantages to providers, including the following:
- Reduced cancellations and no-shows. With telehealth, patients have fewer reasons to cancel or not show up for their appointments. Providers can reach out prior to or at the appointment time to remind the patient of the appointment.
- Encourage better choices. Telehealth provides more ways for providers to communicate about and encourage their patients' healthy lifestyle choices.
- More effective communication. Telehealth helps patients engage with healthcare providers more frequently, giving the provider a fuller view of the patient and a better foundation for treating them. For example, telehealth consultations let the physician see the environment that the patient lives in, which might be useful in treating them.
- Patient education. In addition to receiving more quality health information about the patient, telehealth gives providers more ways to educate patients about their treatment plan.
- Streamlined process. Telehealth can be used to route patients more efficiently to the correct department or specialist and reduce wait times.
- Increased collaboration among departments. Hospitals include a variety of medical disciplines that communicate with each other to serve patients. Telehealth technology facilitates this, enabling departments to share data in ways that yield better results for the patient.
Disadvantages of telehealth
Some of the challenges of telehealth include the following:
- Security risks. Telehealth systems are susceptible to hackers and breaches. Healthcare organizations are one of the biggest targets for online criminals and cybersecurity attacks.
- Regulatory complications. Many states don't allow online prescribing without an established relationship between the physician and patient. In those states, a physical examination or evaluation is required before a physician can write a prescription for a patient, but there are inconsistencies in state laws as to what constitutes a physical examination.
- Technical challenges. Telehealth providers must be trained on how to use telehealth equipment. In addition, there are the costs of the equipment, such as integrated telehealth carts and encounter management software, to consider. The startup cost of implementing telehealth may be especially prohibitive to rural facilities.
- Licensing issues. Certain states require providers who practice telehealth across state lines have a valid license in the state where the patient is located. This means providers must obtain and uphold multiple state licenses.
- Data issues. Depending on the technology used, low bandwidth may affect the accuracy of patient data transmitted, leaving open the potential for misdiagnosis.
Coverage and cost
Telehealth visits often are a less expensive way to provide medical care for both patients and providers. Health insurers often provide financial incentives to encourage patients to make use of telehealth services.
There are a variety of payment models used for telehealth services. Some health systems offer telehealth consultations as part of their regular care services; payers charge patients based on insurance plans or government reimbursement schedules. In other cases, a patient's employer offers a virtual care option as part of health insurance coverage premiums. Some people may opt to independently use a telehealth vendor for a flat fee.
The Centers for Medicare & Medicaid Services expanded telehealth access and reimbursement in the federal Physician Fee Schedule in response to the increased need for telehealth during the COVID-19 pandemic. The public health emergency is set to end on May 11, 2023, as of this writing. Many Medicare telehealth provisions authorized during the public health emergency were extended by the Consolidated Appropriations Act of 2023 through Dec. 31, 2024.
United States telehealth laws
In recent years, many states have passed laws that make telehealth easier to provide. Federal health regulators are exploring ways to extend Medicare reimbursements for telehealth services beyond December 2024.
Although the Patient Protection and Affordable Care Act of 2010 governs telehealth in certain situations under Medicare, telehealth regulation for the most part falls to the states. As of spring 2018, 49 states and the District of Columbia provide reimbursement through Medicaid for some type of live video care, according to the Center for Connected Health Policy, a group that promotes telehealth.
Laws about how prescriptions are issued through telehealth consultations vary by state, as well. The general trend is that more states allow these online prescriptions; however, some states require the establishment of a doctor-patient relationship. Until recently, virtual visits did not qualify as a legitimate doctor-patient relationship in some states.
Telemedicine vs. telehealth
Telemedicine used to be considered a subset of telehealth, but the two terms are now synonymous.
In the past, the label telehealth included nonclinical services, such as continuing medical education, provider training and administrative meetings. In contrast, telemedicine originally only pertained to the use of electronic communications to provide clinical services without requiring a patient to come into a healthcare provider's office or hospital.
The U.S. Federal Communications Commission sometimes uses the term e-care as an umbrella label for any electronic exchange of information that aids in the practice of advanced analytics and medicine.
History of telehealth
The development of modern telehealth began with the invention of the telecommunication technology and infrastructure, including the telephone and telegraph. Early on, telehealth technology was used in military situations. For example, during the Civil War, telegraph messages were used to order medical supplies. Casualty and injury lists were also delivered via telegraph.
The first transfer of a medical image occurred in 1948 in Pennsylvania, when radiology images were sent 24 miles between two townships via telephone line. A few years later, Canadian radiologists created a similar teleradiology system for use in Montreal. In 1959, clinicians at the University of Nebraska transmitted neurological examinations across campus to medical students using two-way interactive television.
Early computer-based patient records were in use in the 1960s. Electronic medical records (EMR), also called electronic health records, started to be more widely used in the 1980s. As part of the American Recovery and Reinvestment Act, healthcare providers were required to show "meaningful use" of EMRs by Jan. 1, 2014, to maintain their Medicare and Medicaid reimbursement levels.
In the early days of telehealth, healthcare professionals used the technology to reach patients living in rural areas. However, the technology quickly expanded into urban areas, especially those that suffered from healthcare shortages.
The future of telehealth
As healthcare providers seek more efficient ways to provide care at less cost to the patient, telehealth's role has grown. The use of virtual healthcare grew during the pandemic. It is likely that telehealth use will continue to grow and be incorporated into the healthcare provision worldwide.
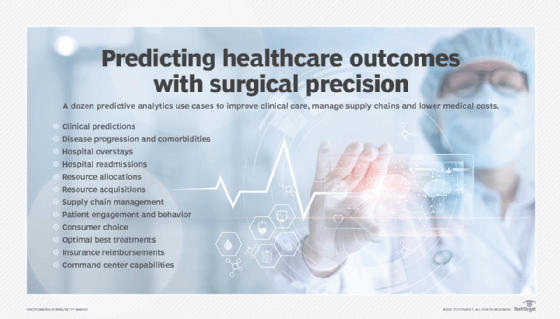
Telehealth will continue to incorporate technologies like artificial intelligence and machine learning to provide predictive healthcare analytics and mine emergent medical data. As telehealth technologies advance, there will be a need for regulatory oversight and reform to ensure patients are protected.
The internet of things (IoT) is likely to play a significant role in the future of telehealth. However, healthcare IoT comes with several cybersecurity risks that endanger patient data. Learn the risks of healthcare IoT and how to mitigate them.




