enterprise master patient index (EMPI)
An enterprise master patient index (EMPI) is a database that is used to maintain consistent and accurate information about each patient registered by a healthcare organization. It may link several smaller MPIs together, such as those from outpatient clinics and rehabilitation facilities. An EMPI can also aggregate patient data contained in separate systems within one facility.
An EMPI ensures that every patient is represented only once, and with constant demographic identification within all systems of hospital data. By keeping this data well-organized, hospitals can provide more efficient and accurate care for their patients.
How does an EMPI work?
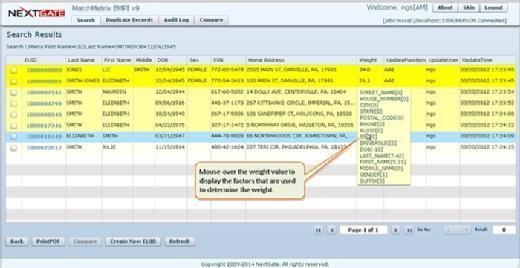
An EMPI uses algorithms to constantly look for duplicate records in a healthcare organization's registration system. The algorithms scan for data elements within the patient's information; for example, their name, address, medical record number, Social Security number, insurance company or healthcare provider.
This technology determines whether records belong to the same patient or if more research is needed.
Algorithms for identifying duplicates
An EMPI uses two algorithms to match patient records: deterministic and probabilistic.
Deterministic matching, also called exact match logic, looks for an exact match of the data elements in a patient record. For example, two records will match if they agree on elements such as the patient's first and last name and phone number. Elements that do not match exactly, such as a nickname or maiden name, will likely cause a rejection.
Probabilistic matching assigns a rank to different data elements based on a preset acceptable level of certainty and scores the likelihood that two or more records belong to the same patient. The higher the score, the higher the probability that there is a match between two records.
Calculating the EMPI error rate
To calculate the EMPI error rate, divide the total number of duplicate patient records in the database by the total number of records multiplied by 100. The average duplicate record rate is approximately 10%, according to the American Health Information Management Association.
Building an EMPI
An EMPI should include patient information, such as their name, date of birth, gender, race, Social Security number, place of residence, email address and phone number. This information provides a clear and complete view of an individual patient, as well as a large-scale view of the demographics with which a healthcare organization is working.
The EMPI may also include a unique identifier to refer to a patient across the entire enterprise, called an enterprise user ID.
Effect of electronic health records on EMPI
An EMPI is often created by and accessed from electronic health record (EHR) systems. However, differences in vendors' EHRs often cause irregularities between EMPIs, and reduce the possibility of a clean health information exchange (HIE). Therefore, maintaining consistency across different EHR systems and EMPIs is essential for reducing medical errors and improving patient care.
Some U.S. health IT leaders believe that a government- or industry-driven national patient identification system would solve this problem, and that it could eventually lead to a national EMPI. Patient data is typically only kept in the EMPIs of hospitals at which they are registered, as well as in the EHRs of the ambulatory providers and specialists they see.
In contrast, the Centers for Medicare and Medicaid Services issued all licensed providers a unique, 10-digit national provider identifier.
Key vendors
EHRs aren't the only healthcare systems that contain an MPI. Lab systems, radiology information systems and computerized physician order entry systems generate unique patient identifiers that can be connected to an MPI.
McKesson, Allscripts Healthcare Solutions and AthenaHealth are a few vendors that sell EMPIs, packaged as part of other products or as stand-alone systems, to healthcare providers.
Because EMPIs store data in the same format, they can function as the source of health information exchange between healthcare facilities. HIEs, in turn, are relied upon in accountable care organization (ACO) settings, as they reduce the amount of work ACOs must do to make sense of and report disparate data collected from the various healthcare organizations participating in the ACO. This arrangement makes the EMPI a key component in enabling health data analytics en route to population health management.
EMPI deployment
An EMPI is commonly deployed in either an active or passive mode.
An active EMPI deployment means the application is used on the front end during patient registration and scheduling. A passive EMPI deployment is used on the back end, with identification occurring after the registration process.
Data integrity
To ensure data integrity, an EMPI must contain only one complete, consistent and accurate record for each patient registered within the healthcare organization.
One of the first steps to ensuring the integrity of patient data is to know what is in the EMPI by analyzing the data to find duplicate records or other errors.
The EMPI can use record-matching algorithms to identify duplicate records; however, some algorithms only identify exact matches, and they can miss duplicates that have small inconsistencies, such as one mistyped digit. It may then be necessary to use advanced algorithms to further identify duplicate records.




